By Jordana Bieze Foster
Parents of local youth and high school athletes got some help navigating the complexities of concussion injuries on Sunday from one of the best known concussion experts in the country, and learned that there are steps parents and coaches can take to minimize young athletes’ risk of serious brain injury.
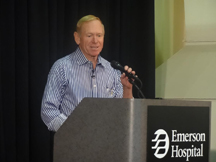
Parents, coaches, and healthcare practitioners packed the cafeteria at Emerson Hospital’s Dr. Robert C. Cantu Concussion Center, which opened its doors in August, to be educated about concussion and its
management by the neurologist for whom the center in Concord Woods Office Park is named.
Scientists’ understanding of concussion is constantly evolving, as evidenced by the fact that the injury’s definition 50 years ago was based on loss of consciousness but now encompasses symptoms even peripherally related to the brain, said Robert C. Cantu, MD, the center’s medical director and director of clinical research. One consistent theme of that evolution is the increasing realization that concussion symptoms and outcomes vary from patient to patient, and parents aren’t wrong to worry about a diagnosis of concussion even if it’s an athlete’s first.
“Concussions are not created equal, and we shouldn’t think of it as a numbers game,” Cantu said. “One concussion may be too many, depending on how long the symptoms last.”
Some of the center’s activity involves adding to the body of research on concussion, including studies that reconstruct the forces involved in helmet-to-helmet collisions or impacts involving a smaller mass, such as a fist, at closer range. But the center also provides clinical services for patients who have sustained sports-related concussions or other traumatic brain injuries.
Patients must be free from symptoms—which include cognitive, mood-related, and sleep-related symptoms in addition to physical symptoms such as headaches—before they can be cleared to return to sports participation. And since research increasingly indicates that returning to activity too soon after a concussion can greatly increase the risk of long-term deficits, the center’s staff works to maximize a recovering athlete’s sport readiness from as many angles as possible.
“If you treat things right, the injured nerve cells have a chance to recover,” Cantu said. “But if you don’t, there’s a chance those cells will die.”
Attendees at Sunday’s event got a first-hand look at two examples of the center’s state-of-the-art rehabilitation equipment.
Occupational therapist Kristen Dixon Kielty demonstrated the Dynavision system, which helps patients improve their ability to respond to signals in their peripheral vision. Not unlike playing a video game, the patient stands in front of a large square board covered with small targets that are programmed to light up at specific intervals; the patient must respond by tapping each light as soon as he or she perceives it in her peripheral vision. As the rehabilitation progresses, the complexity of the task increases.
“This can be a good stepping stone from rehabilitation where an athlete is isolated from the team, to rehab that is more sport-specific,” Kielty said.

Jordana Bieze Foster
In the next room, physical therapist Josh Avery explained the Vasper rehabilitation system, in which patients perform a recumbent cycling exercise with the application of restricted blood flow and cold therapy, a
combination of rehab techniques that trick the body into believing it’s undergoing more intense exercise than it actually is. This can enable patient recovering from concussion to experience the metabolic benefits of intense exercise without risking a setback, Avery said.
But not all aspects of concussion rehabilitation involve expensive equipment, and some of low-tech rehab techniques also can be used to help minimize the risk of concussion in athletes who’ve never had one. Chris Iby, a physical therapist and strength and conditioning specialist at the center, said two particular areas he emphasizes are neck strength and core strength.
“The stronger your foundation is, the more effective it will be at attenuating forces traveling up to the brain,” Iby said. “The neck is the foundation for the head, and the core is the foundation for the neck.”
In both cases, he said, it’s important for strength training to occur in all three planes of movement—frontal (side to side), sagittal (forward and back), and transverse (rotational)—to improve an athlete’s response to impacts from unanticipated directions, which research suggests are associated with increased concussion severity.
Iby also stressed the importance of screening athletes prior to the start of a season to identify any unrecognized concussion-related symptoms as well as potential deficits in strength, balance, eye tracking, and neurocognitive performance that could increase an athlete’s risk for concussion. Ideally teams and school districts would implement this type of screening for all athletes, but in reality that doesn’t always happen; the concussion center offers screening as an out-of-pocket service for parents concerned that their children may fall through the cracks.
No matter who performs it, this type of screening is valuable to establish a baseline for each athlete, so if that athlete does sustain a concussion, his or her rehabilitation can use those baseline values as targets for recovery. But screening may also have preventive benefits; an athlete who undergoes training to address deficits identified during screening will by definition reduce his or her risk of suffering a concussion at all.
“Prevention starts with screening,” Iby said. “If we find anything that needs correction, we can get at it before it becomes an issue.”